The Signs of Pancreatitis
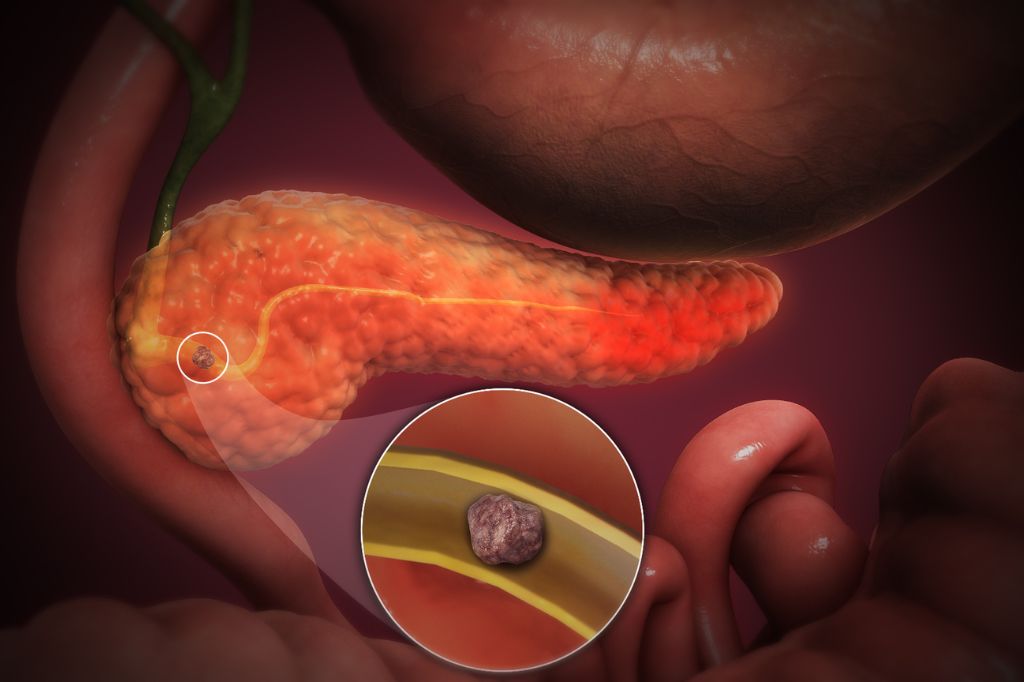
Pancreatitis is something you don’t want to mess around with. It’s when your pancreas, a small but mighty organ responsible for helping you digest food and control your blood sugar, gets inflamed. When this happens, it can lead to some serious health issues. The good news is that your body usually gives you some pretty clear signs when something’s wrong. So, let’s talk about the symptoms of pancreatitis that you need to be on the lookout for.
You Might Feel Sudden, Sharp Abdominal Pain That Shoots to Your Back
If you suddenly get hit with a sharp pain in your upper abdomen, and it feels like it’s stabbing you in the back as well, that’s a red flag. This isn’t just your typical stomach ache. We’re talking about pain that’s so intense it can bring you to your knees and doesn’t go away after a few minutes. It’s like your body is shouting at you that something’s not right. This kind of pain tends to get worse after you eat, especially if you’ve had a greasy meal. If you’re dealing with this, don’t wait it out—get yourself to a doctor right away because it could be a sign of acute pancreatitis, and that’s a big deal.
Nausea and Vomiting That Just Won’t Quit
We’ve all felt nauseous at some point, but when it’s paired with constant vomiting and just won’t let up, it’s time to pay attention. This isn’t the kind of nausea that passes after you lie down for a bit. It sticks around and can really wear you down, especially if it’s accompanied by that sharp abdominal pain I mentioned earlier. If you’re throwing up and can’t keep anything down, it’s definitely time to see a doctor. Your body might be trying to tell you that your pancreas is in trouble.
Fever and an Elevated Heart Rate May Indicate an Infection
If you suddenly spike a fever and your heart feels like it’s running a marathon even though you’re just sitting down, that’s another sign that something’s off. Your body could be fighting an infection or dealing with inflammation, both of which are common with pancreatitis. This isn’t just your run-of-the-mill fever—if you’re also dealing with abdominal pain and nausea, these symptoms are telling you it’s time to take action. Pancreatitis can get worse quickly, so don’t ignore these signs.
Bloating and Tenderness in Your Abdomen Can Be Noticeable
Feeling bloated and noticing that your belly is tender to the touch can be more than just a sign that you ate too much. When your pancreas is inflamed, it can cause your abdomen to swell up, making you feel full and uncomfortable, even if you haven’t eaten much. This kind of bloating isn’t something to brush off, especially if it comes with pain and other symptoms. If your belly is swollen and tender, it’s worth getting it checked out by a doctor.
Yellowish Tint to Your Skin and the Whites of Your Eyes
If you notice that your skin or the whites of your eyes are turning yellow, that’s a sign of jaundice, which can be a big warning signal. Jaundice happens when your pancreas gets so inflamed that it blocks the bile duct, causing a buildup of bilirubin in your body. This yellowing is your body’s way of waving a big red flag that says, “Pay attention!” If you see this, especially along with the other symptoms, don’t wait—get to a doctor immediately.
Unexpected Weight Loss May Be a Warning Sign
The major symptom of pancreatitis is unintentional weight loss. If your pancreas isn’t doing its job, you’re not digesting your food properly, and that can lead to some serious weight loss. You might notice that your clothes are getting looser even though you haven’t changed your diet or exercise routine. If you’re dropping pounds without explanation and you’ve got other symptoms like pain or nausea, it’s time to see a doctor.
Diarrhea and Oily Stools That Just Don’t Seem Normal
Let’s talk about something a bit uncomfortable—your bathroom habits. If you’re dealing with diarrhea or you notice that your stools are oily and foul-smelling, that’s not something to ignore. This can happen when your pancreas isn’t releasing enough enzymes to break down your food, causing undigested fat to pass through your system. While it might seem embarrassing to bring up with your doctor, it’s important. These changes could be a sign of pancreatitis, and the sooner you get it checked out, the better.
So, there you have it—the signs of pancreatitis you need to be aware of. This condition is serious, and if you notice any combination of these symptoms, don’t hesitate to get medical help. The sooner you address it, the better off you’ll be. Pancreatitis isn’t something to take lightly, but with the right attention, you can manage it and protect your health.