Why You Shouldn’t Ignore Rectal Pressure or Pain
What does rectal pressure or pain feel like? Rectal discomfort shows up in different ways. Some people feel a dull heaviness, almost as if something is stuck. Others notice sharp stabs each time they move their bowels. Burning, itching, or throbbing after sitting for long periods can also signal trouble. No matter the exact sensation, your body is sending a message that something needs attention.

Common Everyday Causes
Certain daily habits and conditions trigger mild rectal pain:
- Constipation. Hard stool stretches the anal canal, leading to aching or tearing sensations.
- Hemorrhoids. Swollen veins in the rectum or anus often create pressure and bright-red spotting on toilet paper.
- Anal fissures. Tiny tears in the lining of the anus produce sharp pain during and after bowel movements.
- Proctitis or infections. Bacterial, viral, or inflammatory infections irritate rectal tissue, causing soreness and an urge to pass stool even when the rectum is empty.
- Pelvic floor tension. Tight muscles around the anus can spasm, creating a cramp-like feeling that comes and goes.
These issues respond well to fiber-rich food, adequate water, warm sitz baths, and over-the-counter creams. Even so, monitor symptoms closely.
Conditions That Deserve Urgent Attention
Rectal pain sometimes points toward serious disease:
- Colorectal cancer. A growth inside the rectum can press on local nerves, leading to chronic discomfort. Coupled with bleeding, weight loss, or changes in stool shape, this symptom needs prompt screening.
- Abscesses and fistulas. An infected gland near the anus can fill with pus. Pain worsens quickly, and fever may appear. Untreated abscesses may tunnel to the skin, forming a fistula that leaks fluid.
- Inflammatory bowel disease (IBD). Ulcerative colitis and Crohn’s disease inflame the lining of the large intestine, producing pain, diarrhea, and urgent bowel movements.
- Thrombosed external hemorrhoid. A clot forming within an external hemorrhoid causes sudden, severe pain and a tender, bluish lump.
Any sign of these conditions warrants evaluation without delay. Early treatment lowers complications and improves recovery rates.
Warning Signs You Shouldn’t Ignore
Seek medical care if you experience:
- Bleeding more than a few drops
- Dark or tar-like stool
- Pain lasting longer than one week
- Fever, chills, or night sweats
- Unexplained weight loss or fatigue
- New bowel habit changes, such as ribbon-thin stool
- A palpable mass or external lump that keeps growing
These clues signal that home care is not enough. A healthcare professional must look deeper.
How Do Doctors Know What To Diagnose You With?
Doctors use several reliable tools to uncover the source of rectal pain:
- Detailed history and physical exam. Questions about diet, medications, bowel patterns, and family history guide next steps. A gentle digital rectal exam checks for masses or tenderness.
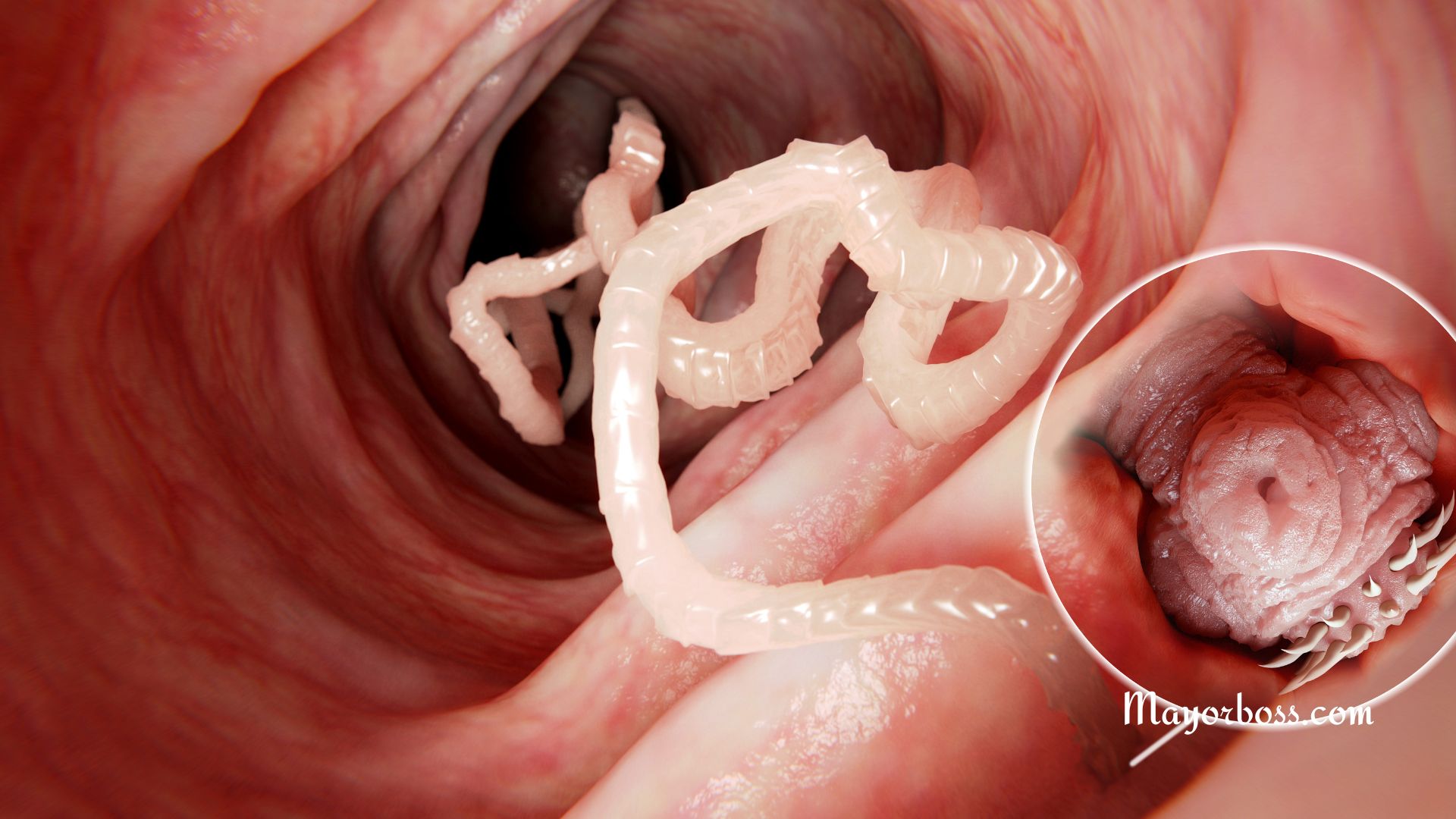
- Anoscopy or sigmoidoscopy. A lighted scope allows direct inspection of the lower bowel lining for fissures, hemorrhoids, or tumors.
- Colonoscopy. If symptoms suggest a disease higher in the colon, a longer scope views the entire large intestine and allows tissue sampling.
- Imaging studies. Ultrasound, CT, or MRI detects deeper abscesses, fistulas, and muscular problems.
- Stool and blood tests. Lab work can identify infection, inflammation markers, or hidden blood.
These steps guide a precise diagnosis, leading to focused treatment.
Treatment
Therapy depends on the underlying cause:
- Lifestyle adjustments. Extra fiber, at least eight cups of water each day, and regular exercise keep stool soft and easy to pass.
- Topical relief. Witch hazel pads, hydrocortisone ointment, or anesthetic gels ease itching and inflammation.
- Warm sitz baths. Ten to fifteen minutes in hip-deep warm water relaxes muscles and improves blood flow to speed healing.
- Prescription medication. Doctors may recommend stool softeners, anti-inflammatory drugs, antibiotics, or suppositories for infection and IBD.
- Minimally invasive procedures. Rubber-band ligation treats troublesome internal hemorrhoids; incision and drainage relieve abscesses.
- Surgery. Persistent fissures, large fistulas, or suspected cancer may need operative repair or removal of diseased tissue.
Everyday Prevention Tips
You cannot prevent every rectal disorder, yet consistent habits lower risk:
- Eat fiber-rich meals. Whole grains, fruits, vegetables, legumes, and nuts add bulk that keeps stool soft.
- Stay hydrated. Water helps fiber do its job and prevents hard stool.
- Move often. Walking or stretching for at least thirty minutes most days stimulates bowel activity and reduces venous pressure.
- Respond to nature’s call promptly. Holding stool for long periods forces the rectum to stretch, which strains tissues.
- Use proper toilet posture. Elevating feet on a small stool unbends the anorectal angle, easing passage.
- Maintain healthy weight. Extra pounds increase pressure on pelvic veins, encouraging hemorrhoid growth.
- Practice gentle hygiene. Fragrance-free wipes and mild soap prevent irritation around the anus.
Small daily choices safeguard long-term rectal health.
Frequently Asked Questions
Can stress cause rectal pain?
Yes. Anxiety increases muscle tension throughout the body, including the pelvic floor. Relaxation techniques such as deep breathing and yoga can reduce flare-ups.
Is rectal bleeding always serious?
Not always. Bright-red spotting from hemorrhoids or fissures is common. However, any bleeding that persists or mixes with stool needs professional evaluation to rule out cancer or IBD.
Will over-the-counter creams cure hemorrhoids?
They relieve soreness and itching but do not remove swollen veins. Lifestyle measures, office procedures, or surgery may still be required for long-term control.